Home » Health Education » Disease Information » Sticky Plaque Treatments Need to Start Earlier Alzheimers
Older adults with evidence of “plaques” in the brain are more likely to see their memory and thinking skills wane over the next few years, a new study finds.
Researchers said the results bolster a long-held theory: The buildup of abnormal proteins in the brain signals an early stage of Alzheimer’s disease.
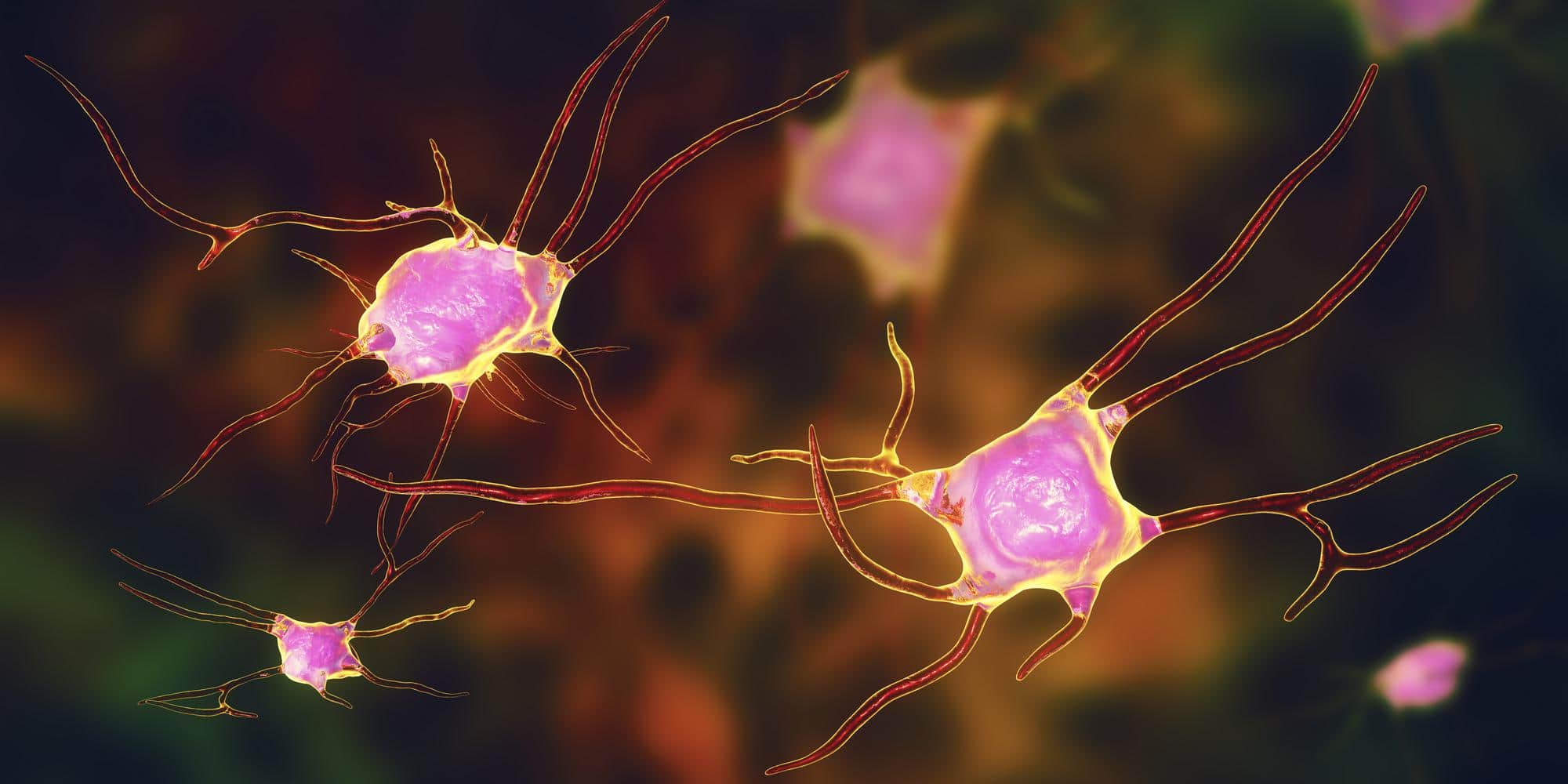
It’s been known for years that in people with Alzheimer’s, the brain accumulates abnormal protein deposits dubbed “plaques” and “tangles.” Plaques are clusters that contain a sticky protein called beta-amyloid.
But even people with no outward signs of dementia can have abnormal beta-amyloid levels in the brain.
In fact, research suggests that’s true of about one-third of adults older than 65, said Dr. Paul Aisen, the senior researcher on the new study.
A major question has been: What does elevated beta-amyloid mean in a dementia-free person?
“There are three broad possibilities,” said Aisen, a professor of neurology at the University of Southern California’s health sciences campus in San Diego. “One is that it means nothing, and it’s just an incidental finding.”
Alternatively, he said, people with increased beta-amyloid may have a heightened risk of eventually developing Alzheimer’s.
The third possibility, Aisen said, is that beta-amyloid buildup is actually an early stage of Alzheimer’s.
The new findings support that third explanation, according to Aisen.
It’s a critical distinction, experts said, because the ultimate hope is to spot people in the earliest stages of Alzheimer’s, when it might be possible to prevent or slow the progression.
To do that, researchers need more than effective treatments. They also need reliable “biomarkers” — signs — that indicate a person is on the path to dementia, explained Heather Snyder, senior director of medical and scientific operations for the Alzheimer’s Association.
A biomarker is something that can be measured to reliably indicate that a disease is present, even if there are no outward symptoms.
“We want to identify people early, and then intervene to change the trajectory of the disease — whether that’s through medication, lifestyle measures or a combination,” said Snyder, who wasn’t involved in the new study.
“We’re not there yet,” she stressed.
But, Snyder said, the new findings add to evidence that the buildup of beta-amyloid “is not a benign process,” and can instead serve as a biomarker.
Researchers are developing a number of experimental drugs aimed at slowing Alzheimer’s — including medications that target beta-amyloid proteins.
In earlier trials, “anti-amyloid” drugs have not panned out, Aisen explained.
But, he said, that may be because the treatments were given too late in the course of the disease.
Some recent research has shown more promise. A trial reported last year found that an anti-amyloid antibody seemed to slow the rate of decline among patients with mild or “pre-clinical” Alzheimer’s, according to the Alzheimer’s Association.
The new study included 445 older U.S. and Canadian adults (average age 74) who had no signs of dementia at the outset. Just over 200 did, however, have elevated levels of beta-amyloid in the brain.
The proteins were detected either in spinal fluid samples, or by specialized PET scans of the brain.
Overall, the study found, people with elevated beta-amyloid showed a steeper decline in their memory and other mental skills over the next three years.
By year four, almost one-third had developed symptoms consistent with the “prodromal” stage of Alzheimer’s — memory issues and other problems that appear before full-blown dementia.
That compared with 15 percent of older adults with normal beta-amyloid levels.
It’s not clear yet how many study participants will eventually develop dementia, Snyder said.
But Aisen said he suspects that, if they live long enough, all older adults with high beta-amyloid will progress to that point.
A small number of study participants have been followed for up to 10 years. Based on their outcomes, the researchers estimated that 88 percent of those with elevated beta-amyloid will have developed mental decline after a decade.
But, the study doesn’t answer one fundamental question: Does the buildup of beta-amyloid actually cause Alzheimer’s?
Aisen believes that the evidence strongly points in that direction.
There is currently no way to prevent Alzheimer’s progression, and doctors don’t test for elevated beta-amyloid in routine practice — it’s only done in research.
Eventually, Snyder said, researchers may find that a combination of biomarkers works best to pinpoint those older adults who can benefit from any preventive therapies that prove effective.
The Alzheimer’s Association was one of the funders of the study, along with the U.S. National Institutes of Health and a list of drug companies that are developing Alzheimer’s therapies. Aisen and several colleagues have received funding or personal fees from those companies.
The study was published June 13 in the Journal of the American Medical Association.
Health Education Articles
Explore our library to stay on top of the latest trends, research, and helpful guidance based on your health needs.
Healthy Living
Stay informed on changes to everyday living that have a big impact on long-term health.
Diet & Nutrition
Get healthy recipes and advice proven to reduce risk of serious illnesses.
Disease Information
Discover the latest research about health issues often addressed by our services.